BP, which is the most common of the subepithelial blistering diseases, occurs chiefly in adults over the age of 60 years; it is self-limited and may last from a few months to 5 years. BP may be a cause of death in older debilitated individuals.
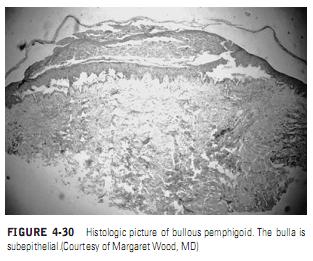
BP has occasionally been reported in conjunction with other diseases, particularly multiple sclerosis and malignancy, or drug therapy, particularly diuretics.In pemphigoid, the initial defect is not intraepithelial as in PV, but it is subepithelial in the lamina lucida region of the basement membrane(Figure 4-30). There is no acantholysis, but the split in the basement membrane is accompanied by an inflammatory infiltrate that is characteristically rich in eosinophils.
Direct immunofluorescent study of a biopsy specimen demonstrates deposition of IgG bound to the basement membrane. Indirect immunoflourescent study of serum obtained from patients with BP demonstrates IgG antibodies bound to the epidermal side of salt-split skin onto antigens that have been named BP antigens 1 and 2. This latter test is particularly useful in distinguishing BP from another subepithelial bullous disease, epidermolysis bullosa aquisita, which has IgG antibodies localized to the dermal side of the salt-split skin.
Clinical Manifestations. The characteristic skin lesion of BP is a blister on an inflamed base that chiefly involves the scalp, arms, legs, axilla, and groin (Figure 4-31). Pruritic macules and papules may also be a presenting sign. The disease is self-limiting but can last for months to years without therapy. Patients with BP may experience one episode or recurrent bouts of lesions. Unlike pemphigus, BP is rarely life threatening since the bullae do not continue to extend at the periphery to form large denuded areas, although death from sepsis or cardiovascular disease secondary to long-term steroid use has been reported to be high in groups of sick elderly patients.Oral Manifestations. Oral involvement is common in BP. Lever reported 33 patients with bullous pemphigoid. Oral lesions were present in 11.In 3 of the cases, the oral lesions preceded the skin lesions, most frequently on the buccal mucosa. Venning and colleagues reported oral lesions in 50% (18 of 36) of BP patients studied.The oral lesions of pemphigoid are smaller, form more slowly, and are less painful than those seen in pemphigus vulgaris, and the extensive labial involvement seen in pemphigus is not present. Desquamative gingivitis has also been reported as a manifestation of BP. The gingival lesions consist of generalized edema, inflammation, and desquamation with localized areas of discrete vesicle formation. The oral lesions are clinically and histologically indistinguishable from
Clinical Manifestations. The characteristic skin lesion of BP is a blister on an inflamed base that chiefly involves the scalp, arms, legs, axilla, and groin (Figure 4-31). Pruritic macules and papules may also be a presenting sign. The disease is self-limiting but can last for months to years without therapy. Patients with BP may experience one episode or recurrent bouts of lesions. Unlike pemphigus, BP is rarely life threatening since the bullae do not continue to extend at the periphery to form large denuded areas, although death from sepsis or cardiovascular disease secondary to long-term steroid use has been reported to be high in groups of sick elderly patients.Oral Manifestations. Oral involvement is common in BP. Lever reported 33 patients with bullous pemphigoid. Oral lesions were present in 11.In 3 of the cases, the oral lesions preceded the skin lesions, most frequently on the buccal mucosa. Venning and colleagues reported oral lesions in 50% (18 of 36) of BP patients studied.The oral lesions of pemphigoid are smaller, form more slowly, and are less painful than those seen in pemphigus vulgaris, and the extensive labial involvement seen in pemphigus is not present. Desquamative gingivitis has also been reported as a manifestation of BP. The gingival lesions consist of generalized edema, inflammation, and desquamation with localized areas of discrete vesicle formation. The oral lesions are clinically and histologically indistinguishable from
oral lesions of mucous membrane pemphigoid, but early remission of BP is more common.
Treatment. Patients with localized lesions of BP may be treated with high-potency topical steroids,whereas patients with severe disease require use of systemic corticosteroids alone or combined with immunosuppressive drugs such as azathioprine, cyclophosphamide, or mycophenolate. Patients with moderate levels of disease may avoid use of systemic steroids by use of dapsone or a combination of tetracycline and nicotinamide.
Treatment. Patients with localized lesions of BP may be treated with high-potency topical steroids,whereas patients with severe disease require use of systemic corticosteroids alone or combined with immunosuppressive drugs such as azathioprine, cyclophosphamide, or mycophenolate. Patients with moderate levels of disease may avoid use of systemic steroids by use of dapsone or a combination of tetracycline and nicotinamide.