General Findings. EM is seen most frequently in children and young adults and is rare after age 50 years. It has an acute or even an explosive onset; generalized symptoms such as fever and malaise appear in severe cases. A patient may be asymptomatic and in less than 24 hours have extensive lesions of the skin and mucosa. EM simplex is a self-limiting form of the disease and is characterized by macules and papules 0.5 to 2 cm in diameter, appearing in a symmetric distribution.
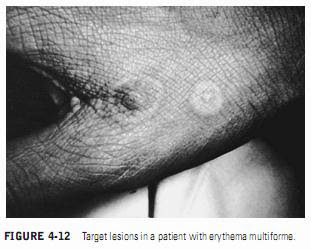
The most common cutaneous areas involved are the hands, feet, and extensor surfaces of the elbows and knees. The face and neck are commonly involved, but only severe cases affect the trunk. Typical skin lesions of EM may be nonspecific macules, papules, and vesicles. More typical skin lesions contain petechiae in the center of the lesion. The pathognomonic lesion is the target or iris lesion, which consists of a central bulla or pale clearing area surrounded by edema and bands of erythema (Figure 4-12).
The more severe vesiculobullous forms of the disease, Stevens-Johnson syndrome and TEN, have a significant mortality rate.
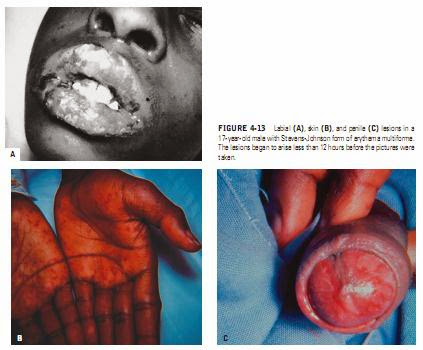
EM is classified as Stevens-Johnson syndrome when the generalized vesicles and bullae involve the skin, mouth, eyes, and genitals
(Figure 4-13). The most severe form of the disease is TEN, (tone epider-
mal neurolysis), which is usually secondary to a drug reaction and results in sloughing of skin and mucosa in large sheets. Morbidity, which occurs in 30 to 40% of patients, results from secondary infection, fluid and electrolyte imbalance, or involvement of the lung, liver, or kidneys.
Patients with this form of the disease are most successfully managed in burn centers, where necrotic skin is removed under general anesthesia and healing takes place under sheets of porcine xenografts.
Oral Findings. Oral lesions commonly appear along with skin lesions in approximately 70% of EM patients
(Figure 4-14). In some cases, oral lesions are the predominant or single site of disease. When the oral lesions predominate and no target lesions are present on the skin, EM must be differentiated from other causes of acute multiple ulcers, especially primary herpes simplex infection. This distinction is important because corticosteroids may be the treatment of choice in EM, but they are specifically contraindicated in primary herpes simplex infections. When there are no skin lesions and the oral lesions are mild, diagnosis may be difficult and is usually made by exclusion of other diseases. Cytologic smears and virus isolation may be done to eliminate the possibility of primary herpes infection. Biopsy may be performed when acute pemphigus is suspected. The histologic picture of oral EM is not considered specific, but the finding of a perivascular lymphocytic infiltrate and epithelial edema and hyperplasia is considered suggestive of EM.
The diagnosis is made on the basis of the total clinical picture, including the rapid onset of lesions. The oral lesions start as bullae on an erythematous base, but intact bullae are rarely seen by the clinician because they break rapidly into irregular ulcers. Viral lesions are small, round, symmetric, and shallow, but EM lesions are larger, irregular, deeper, and often bleed. Lesions may occur anywhere on the oral mucosa with EM, but involvement of the lips is especially prominent, and gingival involvement is rare. This is an important criterion for distinguishing EM from primary herpes simplex infection, in which generalized gingival involvement is characteristic.
In full-blown clinical cases, the lips are extensively eroded, and large portions of the oral mucosa are denuded of epithelium. The patient cannot eat or even swallow and drools blood-tinged saliva. Within 2 or 3 days the labial lesions begin to crust. Healing occurs within 2 weeks in a majority of cases, but, in some severe cases, extensive disease may continue for several weeks.
REATMENT
Mild cases of oral EM may be treated with supportive measures only, including topical anesthetic mouthwashes and a soft or liquid diet. Moderate to severe oral EM may be treated with a
short course of systemic corticosteroids in patients without significant contraindications to their use. Systemic corticosteroids should only be used by clinicians familiar with the side effects, and, in each case, potential benefits should be carefully weighed
against potential risks. Young children treated with systemic steroids for EM appear to have a higher rate of complications than do adults, particularly gastrointestinal bleeding and secondary infections. Adults treated with short-term systemic steroids have a low rate of complications and a shorter course of EM.
The protein-wasting and adrenal-suppressive effects of systemic steroids are not significant when used short-term, and the clinical course of the disease may be shortened. An initial dose of 30 mg/d to 50 mg/d of prednisone or methylprednisolone for several days, which is then tapered, is helpful in shortening the healing time of EM, particularly when therapy is started early in the course of the disease. It should be noted that the efficacy of this treatment has not been proven by controlled clinical trials and is controversial.
Patients with severe cases of recurrent EM have been treated with dapsone, azathioprine, levamisole, or thalidomide. EM triggered by progesterone, also referred to as autoimmune progesterone dermatitis and stomatitis, has been treated successfully with tamoxifen. In resistant cases, oophorectomy has been necessary to cure the disorder.
Antiherpes drugs such as acyclovir or valacyclovir can be effective in preventing susceptible patients from developing herpes associated EM, if the drug is administered at the onset of the recurrent HSV lesion. Prophylactic use of antiherpes drugs is effective in preventing frequent recurrent episodes of HSVassociated EM.
Systemic steroids are recommended for management of Stevens-Johnson syndrome and are considered life saving in severe cases.
EM is classified as Stevens-Johnson syndrome when the generalized vesicles and bullae involve the skin, mouth, eyes, and genitals
(Figure 4-13). The most severe form of the disease is TEN, (tone epider-
mal neurolysis), which is usually secondary to a drug reaction and results in sloughing of skin and mucosa in large sheets. Morbidity, which occurs in 30 to 40% of patients, results from secondary infection, fluid and electrolyte imbalance, or involvement of the lung, liver, or kidneys.
Patients with this form of the disease are most successfully managed in burn centers, where necrotic skin is removed under general anesthesia and healing takes place under sheets of porcine xenografts.
Oral Findings. Oral lesions commonly appear along with skin lesions in approximately 70% of EM patients
(Figure 4-14). In some cases, oral lesions are the predominant or single site of disease. When the oral lesions predominate and no target lesions are present on the skin, EM must be differentiated from other causes of acute multiple ulcers, especially primary herpes simplex infection. This distinction is important because corticosteroids may be the treatment of choice in EM, but they are specifically contraindicated in primary herpes simplex infections. When there are no skin lesions and the oral lesions are mild, diagnosis may be difficult and is usually made by exclusion of other diseases. Cytologic smears and virus isolation may be done to eliminate the possibility of primary herpes infection. Biopsy may be performed when acute pemphigus is suspected. The histologic picture of oral EM is not considered specific, but the finding of a perivascular lymphocytic infiltrate and epithelial edema and hyperplasia is considered suggestive of EM.
The diagnosis is made on the basis of the total clinical picture, including the rapid onset of lesions. The oral lesions start as bullae on an erythematous base, but intact bullae are rarely seen by the clinician because they break rapidly into irregular ulcers. Viral lesions are small, round, symmetric, and shallow, but EM lesions are larger, irregular, deeper, and often bleed. Lesions may occur anywhere on the oral mucosa with EM, but involvement of the lips is especially prominent, and gingival involvement is rare. This is an important criterion for distinguishing EM from primary herpes simplex infection, in which generalized gingival involvement is characteristic.
In full-blown clinical cases, the lips are extensively eroded, and large portions of the oral mucosa are denuded of epithelium. The patient cannot eat or even swallow and drools blood-tinged saliva. Within 2 or 3 days the labial lesions begin to crust. Healing occurs within 2 weeks in a majority of cases, but, in some severe cases, extensive disease may continue for several weeks.
REATMENT
Mild cases of oral EM may be treated with supportive measures only, including topical anesthetic mouthwashes and a soft or liquid diet. Moderate to severe oral EM may be treated with a
short course of systemic corticosteroids in patients without significant contraindications to their use. Systemic corticosteroids should only be used by clinicians familiar with the side effects, and, in each case, potential benefits should be carefully weighed
against potential risks. Young children treated with systemic steroids for EM appear to have a higher rate of complications than do adults, particularly gastrointestinal bleeding and secondary infections. Adults treated with short-term systemic steroids have a low rate of complications and a shorter course of EM.
The protein-wasting and adrenal-suppressive effects of systemic steroids are not significant when used short-term, and the clinical course of the disease may be shortened. An initial dose of 30 mg/d to 50 mg/d of prednisone or methylprednisolone for several days, which is then tapered, is helpful in shortening the healing time of EM, particularly when therapy is started early in the course of the disease. It should be noted that the efficacy of this treatment has not been proven by controlled clinical trials and is controversial.
Patients with severe cases of recurrent EM have been treated with dapsone, azathioprine, levamisole, or thalidomide. EM triggered by progesterone, also referred to as autoimmune progesterone dermatitis and stomatitis, has been treated successfully with tamoxifen. In resistant cases, oophorectomy has been necessary to cure the disorder.
Antiherpes drugs such as acyclovir or valacyclovir can be effective in preventing susceptible patients from developing herpes associated EM, if the drug is administered at the onset of the recurrent HSV lesion. Prophylactic use of antiherpes drugs is effective in preventing frequent recurrent episodes of HSVassociated EM.
Systemic steroids are recommended for management of Stevens-Johnson syndrome and are considered life saving in severe cases.