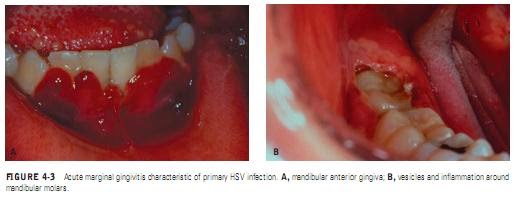
The diagnosis of primary herpetic gingivostomatitis is straightforward when patients present with a typical clinical picture of generalized symptoms followed by an eruption of oral vesicles, round shallow symmetric oral ulcers, and acute marginal gingivitis. Laboratory tests are rarely required in these cases. Other patients, especially adults, may have a less typical clinical picture, making the diagnosis more difficult. This is especially important when distinguishing primary herpes from erythema multiforme since proper therapy differs significantly.
The following laboratory tests are helpful in the diagnosis of a primary herpes infection.
Cytology. For cytology, a fresh vesicle can be opened and a scraping made from the base of the lesion and placed on a microscope slide. The slide may be stained with Giemsa, Wright’s, or Papanicolaou’s stain and searched for multinucleated giant cells (Figure 4-5), syncytium, and ballooning degeneration of the nucleus. Fluorescent staining of cytology smears has been shown to be more sensitive (83%) compared with routine cytology (54%); it is the cytologic test of choice, when available.
HSV Isolation. Isolation and neutralization of a virus in tissue culture is the most positive method of identification and has a specificity and sensitivity of 100%.
HSV Isolation. Isolation and neutralization of a virus in tissue culture is the most positive method of identification and has a specificity and sensitivity of 100%.
A clinician must remember that isolation of HSV from oral lesions does not necessarily mean that HSV caused the lesions. Patients who have lesions from other causes may also be asymptomatic shedders of HSV.
Antibody Titers. Conclusive evidence of a primary HSV infection includes testing for complement-fixing or neutralizing antibody in acute and convalescent sera. However, it is rarely necessary in routine clinical situations and is often not helpful since the results are not available until the infection is gone. In special circumstances, such as immunocompromised
patients, an acute serum specimen should be obtained within 3 or 4 days of the onset of symptoms. The absence of detectable antibodies plus the isolation of HSV from lesions is compatible with the presence of a primary HSV infection. Antibody to HSV will begin to appear in a week and reach a peak in 3 weeks. A convalescent serum can confirm the diagnosis of primary HSV infection by demonstrating at least a fourfold rise in anti-HSV antibody. If anti-HSV antibody titers are similar in both the acute and convalescent sera, then the lesions from which HSV was isolated were recurrent lesions.