Magnetic resonance imaging (MRI) uses electrical and magnetic fields and radiofrequency (RF) pulses, rather than ionizing radiation, to produce an image. The patient is placed within a large circular magnet that causes the hydrogen protons of the body to be aligned with the magnetic field. At this point, energy in the form of RF pulses is added to the system, and the equilibrium is destabilized, with the protons altering their orientation and magnetic moment. After the RF pulse is removed, the protons gradually return to equilibrium, giving up the excess energy in the form of a radio signal that can be detected and converted to a visible image. This return to equilibrium is called relaxation, and the time that it takes is dependent on tissue type. “T1 relaxation” describes the release of energy from the proton to its immediate environment, and “T2 relaxation” designates the interaction between adjacent protons. This whole sequence of applying RF pulses and then picking up the returning signal later is repeated many times in forming the image.
By manipulating the time of repetition (TR) of the pulses and the time of signal detection (time of echo [TE]), the various tissues can be highlighted, allowing the determination of tissue characteristics. For example, when both TR and TE are short (eg, 500 ms/20 ms), the image contrast is due primarily to differences in T1 relaxation times (ie, T1-weighted image) (Figure 3-10, A). Fat produces a bright signal whereas fluids and muscle produce an intermediate signal. If the parameters are adjusted so that both TR and TE are long (2,000 ms/80 ms—a T2-weighted image), fluids become bright and fat
becomes darker (see Figure 3-10, B). By running a variety of different sequences, significant information about tissue character can be obtained. The addition of an intravenous contrast agent (gadolinium-diethylenetriamine pentaacetic acid [DTPA]) allows even more tissue differentiation because certain tumors enhance (ie, produce a brighter signal) in a characteristic way due to increased blood flow.
Similarly to CT, MRI produces images of thin slices of tissue in a wide variety of planes, including oblique angles. Quasidynamic motion studies can also be performed, as can threedimensional reconstruction.
MRI is used primarily for evaluating soft tissues because bone always produces a low signal (black) due to a relative paucity of hydrogen protons. While some information about osseous tissue can be obtained (particularly about alterations in the bone marrow), detailed study of bone is usually reserved for CT. Due to signals emanating from flowing blood, MRI can also be used to evaluate blood vessels, with differentiation between arteries and veins possible. Three-dimensional magnetic resonance (MR) angiography can rival conventional angiography in detail but without the need for the injection of a contrast medium.
Although MRI was first introduced clinically for the evaluation of the brain, it is now used throughout the body, not only for soft tissue but also for the assessment of joints since ligaments (both intact and torn), menisci, surface cartilage, bone marrow abnormalities, and synovial membrane proliferation can all be studied with MRI.
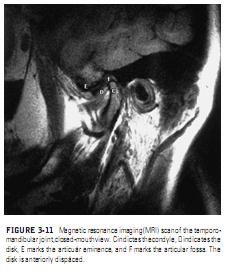
In dentistry, the primary uses of MRI have been the evaluation of various pathologic lesions (such as tumors) and the assessment of the TMJ. A number of cadaver and clinical studies have demonstrated that MRI can accurately depict the location, morphology, and function of the articular disk, thus
allowing the diagnosis of internal derangement to be made or confirmed
(Figure 3-11). Information on joint effusion and pannus formation can also be obtained, and some osseous changes can also be evaluated.
Recent reports have also described the correlation of MR appearance with histology in cases of bone marrow edema or necrosis.
Similarly to CT, MRI produces images of thin slices of tissue in a wide variety of planes, including oblique angles. Quasidynamic motion studies can also be performed, as can threedimensional reconstruction.
MRI is used primarily for evaluating soft tissues because bone always produces a low signal (black) due to a relative paucity of hydrogen protons. While some information about osseous tissue can be obtained (particularly about alterations in the bone marrow), detailed study of bone is usually reserved for CT. Due to signals emanating from flowing blood, MRI can also be used to evaluate blood vessels, with differentiation between arteries and veins possible. Three-dimensional magnetic resonance (MR) angiography can rival conventional angiography in detail but without the need for the injection of a contrast medium.
Although MRI was first introduced clinically for the evaluation of the brain, it is now used throughout the body, not only for soft tissue but also for the assessment of joints since ligaments (both intact and torn), menisci, surface cartilage, bone marrow abnormalities, and synovial membrane proliferation can all be studied with MRI.
In dentistry, the primary uses of MRI have been the evaluation of various pathologic lesions (such as tumors) and the assessment of the TMJ. A number of cadaver and clinical studies have demonstrated that MRI can accurately depict the location, morphology, and function of the articular disk, thus
allowing the diagnosis of internal derangement to be made or confirmed
(Figure 3-11). Information on joint effusion and pannus formation can also be obtained, and some osseous changes can also be evaluated.
Recent reports have also described the correlation of MR appearance with histology in cases of bone marrow edema or necrosis.
The typical MRI examination of the TMJ consists of both closed- and open-mouth views in an oblique sagittal plane, with the sections oriented perpendicular to the long axis of the condyle. Some institutions also routinely obtain images in the coronal plane for easier identification of a lateral or medial displacement of the disk.
The sagittal images are used to evaluate disk position with respect to the head of the condyle. The disk is considered to be in a normal location when the posterior band is superior to the condyle (the so-called twelve-o’clock position) when the mouth is closed, but there is not complete agreement about how far the disk must be from twelve o’clock before anterior displacement is diagnosed.
16
Because there can also be a rotational component to the disk displacement, all slices through the joint should be evaluated, not just the ones that show the disk most clearly. In the open-mouth views, the disk can be seen to be interposed between the condyle and articular eminence (normal or reducing) or to remain anterior to the condyle (nonreducing).
MRI has many advantages over other imaging techniques, including the capability of imaging soft tissue in virtually any plane. It also uses no ionizing radiation and is thus generally considered safe although there are limits on the magnitude of the magnetic field used and although animal studies have shown teratogenicity resulting from MRI in pregnant mice.
The major disadvantage of MRI is its cost, which is typically more than $1,000 per examination. Not only are the equipment, physical facility, and supplies (such as cryogens for the supercooled magnet) costly, the procedure also requires specially trained technologists and radiologists.
MRI is contraindicated for certain patients, including those with demand-type cardiac pacemakers, due to interference by the electrical and magnetic fields. Patients with ferromagnetic metallic objects in strategic places (such as aneurysm clips in the brain and metallic fragments in the eye) also should not be placed in the magnet. Most machines have weight and girth limits for patients because of the size of the bore of the magnet. Some patients feel claustrophobic inside the magnet and may need to be sedated for the procedure. Because of the length of time for each scan in the series (typically several minutes), patients who cannot remain motionless are not good candidates for MRI.
The sagittal images are used to evaluate disk position with respect to the head of the condyle. The disk is considered to be in a normal location when the posterior band is superior to the condyle (the so-called twelve-o’clock position) when the mouth is closed, but there is not complete agreement about how far the disk must be from twelve o’clock before anterior displacement is diagnosed.
16
Because there can also be a rotational component to the disk displacement, all slices through the joint should be evaluated, not just the ones that show the disk most clearly. In the open-mouth views, the disk can be seen to be interposed between the condyle and articular eminence (normal or reducing) or to remain anterior to the condyle (nonreducing).
MRI has many advantages over other imaging techniques, including the capability of imaging soft tissue in virtually any plane. It also uses no ionizing radiation and is thus generally considered safe although there are limits on the magnitude of the magnetic field used and although animal studies have shown teratogenicity resulting from MRI in pregnant mice.
The major disadvantage of MRI is its cost, which is typically more than $1,000 per examination. Not only are the equipment, physical facility, and supplies (such as cryogens for the supercooled magnet) costly, the procedure also requires specially trained technologists and radiologists.
MRI is contraindicated for certain patients, including those with demand-type cardiac pacemakers, due to interference by the electrical and magnetic fields. Patients with ferromagnetic metallic objects in strategic places (such as aneurysm clips in the brain and metallic fragments in the eye) also should not be placed in the magnet. Most machines have weight and girth limits for patients because of the size of the bore of the magnet. Some patients feel claustrophobic inside the magnet and may need to be sedated for the procedure. Because of the length of time for each scan in the series (typically several minutes), patients who cannot remain motionless are not good candidates for MRI.