THE PATIENT WITH CHRONIC MULTIPLE LESIONS
Patients with chronic multiple lesions are frequently misdiagnosed for weeks to months since their lesions may be confused with recurring oral mucosal disorders. The clinician can avoid misdiagnosis by carefully questioning the patient on the initial visit regarding the natural history of the lesions. In recurring disorders such as severe aphthous stomatitis, the patient may experience continual ulceration of the oral mucosa, but individual lesions heal and new ones form. In the
category of disease described in this section, the same lesions are present for weeks to months. The major diseases in this group are pemphigus vulgaris, pemphigus vegetans, bullous pemphigoid, mucous membrane pemphigoid, linear IgA disease, and erosive lichen planus. Herpes simplex infections may cause chronic lesions in patients immunocompromised by cancer chemotherapy, immunosuppressive drugs, or HIV infection.Patients with chronic multiple lesions are frequently misdiagnosed for weeks to months since their lesions may be confused with recurring oral mucosal disorders. The clinician can avoid misdiagnosis by carefully questioning the patient on the initial visit regarding the natural history of the lesions. In recurring disorders such as severe aphthous stomatitis, the patient may experience continual ulceration of the oral mucosa, but individual lesions heal and new ones form. In the
Pemphigus
Pemphigus is a potentially life-threatening disease that causes blisters and erosions of the skin and mucous membranes. These epithelial lesions are a result of autoantibodies that react with desmosomal glycoproteins that are present on the cell surface of the keratinocyte. The immune reaction against these glycoproteins causes a loss of cell-to-cell adhesion, resulting in the formation of intraepithelial bullae.There are 0.5 to 3.2 cases reported each year per 100,000 population, with the highest incidence occurring in the fifth and sixth decades of life, although rare cases have been reported in children and the elderly.Pemphigus occurs more frequently in the Jewish population, particularly among Ashkenazi Jews, in whom studies have shown a strong association with major histocompatibility complex (MHC) class II alleles HLA-DR4 and DQW3. Familial pemphigus has also been reported.
The major variants of pemphigus are pemphigus vulgaris (PV), pemphigus vegetans, pemphigus foliaceus, pemphigus erythematosus, paraneoplastic pemphigus (PNPP), and drugrelated pemphigus. Pemphigus vegetans is a variant of pemphigus vulgaris, and pemphigus erythematosus is a variant of pemphigus foliaceus. Each form of this disease has antibodies directed against different target cell surface antigens, resulting in a lesion forming in different layer of the epithelium. In pemphigus foliaceus, the blister occurs in the superficial granular cell layer, whereas, in pemphigus vulgaris, the lesion is deeper, just above the basal cell layer. Mucosal involvement is not a feature of the foliaceus and erythematous forms of the disease.
PEMPHIGUS VULGARIS
PV is the most common form of pemphigus, accounting for over 80% of cases. The underlying mechanism responsible for causing the intraepithelial lesion of PV is the binding of IgG autoantibodies to desmoglein 3, a transmembrane glycoprotein adhesion molecule present on desmosomes. The presence of desmoglein 1 autoantibodies is a characteristic of pemphigus foliaceus, but these antibodies are also detected in patients with long-standing PV. Evidence for the relationship of the IgG autoantibodies to PV lesion formation includes studies demonstrating the formation of blisters on the skin of mice after passive transfer of IgG from patients with PV.
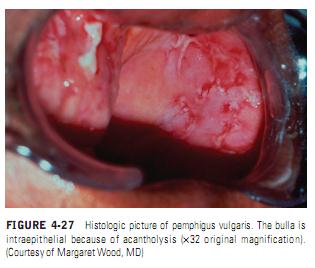
The mechanism by which antidesmoglein antibodies cause the loss of cell-to-cell adhesion is controversial. Some investigators believe that binding of the PV antibody activates proteases, whereas more recent evidence supports the theory that the PV antibodies directly block the adhesion function of the desmogleins.The separation of cells, called acantholysis, takes place in the lower layers of the stratum spinosum (Figure 4-27). Electron microscopic observations show the earliest epithelial changes as a loss of intercellular cement substance; this is followed by a widening of intercellular spaces, destruction of desmosomes, and finally cellular degeneration. This progressive acantholysis results in the classic suprabasilar bulla, which involves increasingly greater areas of epithelium, resulting in loss of large areas of skin and mucosa.
Pemphigus has been reported coexisting with other autoimmune diseases, particularly myasthenia gravis.
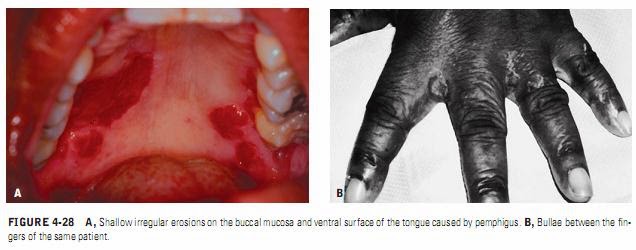
Patients with thymoma also have a higher incidence of pemphigus. Several cases of pemphigus have been reported in patients with multiple autoimmune disorders or those with neoplasms such as lymphoma. Death occurs most frequently in elderly patients and in patients requiring high doses of corticosteroids who develop infections and bacterial septicemia, most notably from Staphylococcus aureus.Clinical Manifestations. The classical lesion of pemphigus is a thin-walled bulla arising on otherwise normal skin or mucosa. The bulla rapidly breaks but continues to extend peripherally, eventually leaving large areas denuded of skin (Figure 4-28). A characteristic sign of the disease may be obtained by application of pressure to an intact bulla. In patients with PV, the bulla enlarges by extension to an apparently normal surface. Another characteristic sign of the disease is that pressure to an appar
ently normal area results in the formation of a new lesion. This phenomenon, called the Nikolsky sign, results from the upper layer of the skin pulling away from the basal layer. The Nikolsky sign is most frequently associated with pemphigus but may also occur in epidermolysis bullosa.
Some patients with pemphigus develop acute fulminating disease, but, in most cases, the disease develops more slowly, usually taking months to develop to its fullest extent.
Oral Manifestations. Eighty to ninety percent of patients with pemphigus vulgaris develop oral lesions sometime during the course of the disease, and, in 60% of cases, the oral lesions are the first sign.
153
The oral lesions may begin as the classic bulla on a noninflamed base; more frequently, the clinician sees shallow irregular ulcers because the bullae rapidly break. A thin layer of epithelium peels away in an irregular pattern, leaving a denuded base. The edges of the lesion continue to extend peripherally over a period of weeks until they involve large portions of the oral mucosa. Most commonly the lesions start on the buccal mucosa, often in areas of trauma along the occlusal plane. The palate and gingiva are other common sites of involvement.
154
It is common for the oral lesions to be present up to 4 months before the skin lesions appear. If treatment is instituted during this time, the disease is easier to control, and the chance for an early remission of the disorder is enhanced. Frequently, however, the initial diagnosis is missed, and the lesions are misdiagnosed as herpes infection or candidiasis. Zegarelli and Zegarelli studied 26 cases of intraoral PV. The average time from onset of the disease to diagnosis was 6.8 months.
155
They also noted that several patients had coexisting candidiasis, which sometimes masked the typical clinical picture of the pemphigus lesions. There is also a subgroup of pemphigus patients whose disease remains confined to the oral mucosa. These patients often have negative results on direct immunofluorescence (DIF).
If a proper history is taken, the clinician should be able to distinguish the lesions of pemphigus from those caused by acute viral infections or erythema multiforme because of the acute nature of the latter diseases. It is also important for the clinician to distinguish pemphigus lesions from those in the RAS category. RAS lesions may be severe, but individual lesions heal and recur. In pemphigus, the same lesions continue to extend peripherally over a period of weeks to months. Lesions of pemphigus are not round and symmetric like RAS lesions but are shallow and irregular and often have detached epithelium at the periphery (see Figure 4-27). In early stages of the disease, the sliding away of the oral epithelium resembles skin peeling after a severe sunburn. In some cases, the lesions may start on the gingiva and be called desquamative gingivitis. It should be remembered that desquamative gingivitis is not a diagnosis in itself; these lesions must be biopsied to rule out the possibility of PV as well as bullous pemphigoid, mucous membrane pemphigoid, and erosive lichen planus.
Laboratory Tests. PV is diagnosed by biopsy. Biopsies are best done on intact vesicles and bullae less than 24 hours old; however, because these lesions are rare on the oral mucosa, the
Some patients with pemphigus develop acute fulminating disease, but, in most cases, the disease develops more slowly, usually taking months to develop to its fullest extent.
Oral Manifestations. Eighty to ninety percent of patients with pemphigus vulgaris develop oral lesions sometime during the course of the disease, and, in 60% of cases, the oral lesions are the first sign.
153
The oral lesions may begin as the classic bulla on a noninflamed base; more frequently, the clinician sees shallow irregular ulcers because the bullae rapidly break. A thin layer of epithelium peels away in an irregular pattern, leaving a denuded base. The edges of the lesion continue to extend peripherally over a period of weeks until they involve large portions of the oral mucosa. Most commonly the lesions start on the buccal mucosa, often in areas of trauma along the occlusal plane. The palate and gingiva are other common sites of involvement.
154
It is common for the oral lesions to be present up to 4 months before the skin lesions appear. If treatment is instituted during this time, the disease is easier to control, and the chance for an early remission of the disorder is enhanced. Frequently, however, the initial diagnosis is missed, and the lesions are misdiagnosed as herpes infection or candidiasis. Zegarelli and Zegarelli studied 26 cases of intraoral PV. The average time from onset of the disease to diagnosis was 6.8 months.
155
They also noted that several patients had coexisting candidiasis, which sometimes masked the typical clinical picture of the pemphigus lesions. There is also a subgroup of pemphigus patients whose disease remains confined to the oral mucosa. These patients often have negative results on direct immunofluorescence (DIF).
If a proper history is taken, the clinician should be able to distinguish the lesions of pemphigus from those caused by acute viral infections or erythema multiforme because of the acute nature of the latter diseases. It is also important for the clinician to distinguish pemphigus lesions from those in the RAS category. RAS lesions may be severe, but individual lesions heal and recur. In pemphigus, the same lesions continue to extend peripherally over a period of weeks to months. Lesions of pemphigus are not round and symmetric like RAS lesions but are shallow and irregular and often have detached epithelium at the periphery (see Figure 4-27). In early stages of the disease, the sliding away of the oral epithelium resembles skin peeling after a severe sunburn. In some cases, the lesions may start on the gingiva and be called desquamative gingivitis. It should be remembered that desquamative gingivitis is not a diagnosis in itself; these lesions must be biopsied to rule out the possibility of PV as well as bullous pemphigoid, mucous membrane pemphigoid, and erosive lichen planus.
Laboratory Tests. PV is diagnosed by biopsy. Biopsies are best done on intact vesicles and bullae less than 24 hours old; however, because these lesions are rare on the oral mucosa, the
biopsy specimen should be taken from the advancing edge of the lesion, where areas of characteristic suprabasilar acantholysis may be observed by the pathologist. Specimens taken from the center of a denuded area are nonspecific histologically as well as clinically. Sometimes several biopsies are necessary before the correct diagnosis can be made. If the patient shows a positive Nikolsky sign, pressure can be placed on the mucosa to produce a new lesion; biopsy may be done on this fresh lesion.
A second biopsy, to be studied by DIF, should be performed whenever pemphigus is included in the differential diagnosis. This study is best performed on a biopsy specimen that is obtained from clinically normal-appearing perilesional mucosa or skin. In this technique for DIF, fluorescein-labeled antihuman immunoglobulins are placed over the patient’s tissue specimen. In cases of PV, the technique will detect antibodies, usually IgG and complement, bound to the surface of the keratinocytes.
Indirect immunofluorescent antibody tests have been described that are helpful in distinguishing pemphigus from pemphigoid and other chronic oral lesions and in following the progress of patients treated for pemphigus. In this technique, serum from a patient with bullous disease is placed over a prepared slide of an epidermal structure (usually monkey esophagus). The slide is then overlaid with fluorescein-tagged antihuman gamma globulin. Patients with pemphigus vulgaris have antikeratinocyte antibodies against intercellular substances that show up under a fluorescent microscope. The titer of the antibody has been directly related to the level of clinical disease. An ELISA (enzyme-linked immunosorbent assay) has been developed that can detect desmoglein 1 and 3 in serum samples of patients with PV. These laboratory tests should provide a new tool for the accurate diagnosis of PV and may also prove useful in monitoring the progress of the disease.
A second biopsy, to be studied by DIF, should be performed whenever pemphigus is included in the differential diagnosis. This study is best performed on a biopsy specimen that is obtained from clinically normal-appearing perilesional mucosa or skin. In this technique for DIF, fluorescein-labeled antihuman immunoglobulins are placed over the patient’s tissue specimen. In cases of PV, the technique will detect antibodies, usually IgG and complement, bound to the surface of the keratinocytes.
Indirect immunofluorescent antibody tests have been described that are helpful in distinguishing pemphigus from pemphigoid and other chronic oral lesions and in following the progress of patients treated for pemphigus. In this technique, serum from a patient with bullous disease is placed over a prepared slide of an epidermal structure (usually monkey esophagus). The slide is then overlaid with fluorescein-tagged antihuman gamma globulin. Patients with pemphigus vulgaris have antikeratinocyte antibodies against intercellular substances that show up under a fluorescent microscope. The titer of the antibody has been directly related to the level of clinical disease. An ELISA (enzyme-linked immunosorbent assay) has been developed that can detect desmoglein 1 and 3 in serum samples of patients with PV. These laboratory tests should provide a new tool for the accurate diagnosis of PV and may also prove useful in monitoring the progress of the disease.
Treatment .
An important aspect of patient management is early diagnosis, when lower doses of medication can be used for shorter periods of time to control the disease. The mainstay of treatment remains high doses of systemic corticosteroids, usually given in dosages of 1 to 2 mg/kg/d. When
steroids must be used for long periods of time, adjuvants such as azathioprine or cyclophosphamide are added to the regimen to reduce the complications of long-term corticosteroid therapy. Prednisone is used initially to bring the disease under control, and, once this is achieved, the dose of prednisone is decreased to the lowest possible maintenance levels. Patients with only oral involvement also may need lower doses of prednisone for shorter periods of time, so the clinician should weigh the potential benefits of adding adjuvant therapy against the risks of additional complications such as blood dyscrasias, hepatitis, and an increased risk of malignancy later in life. There is no one accepted treatment for pemphigus confined to the mouth, but one 5-year follow -up study of the treatment of oral pemphigus showed no additional benefit of adding cyclophosphamide or cyclosporine to prednisone versus prednisone alone, and it showed a higher rate of complications in the group taking the immunosuppressive drug.Most studies of pemphigus of the skin show a decreased mortality rate when adjuvant therapy is given along with prednisone.One new immunosuppressive drug, mycophenolate, has been effective when managing patients resistant to other adjuvants.The need for systemic steroids may be lowered further in cases of oral pemphigus by combining topical with systemic steroid therapy, either by allowing the prednisone tablets to dissolve slowly in the mouth before swallowing or by using potent topical steroid creams. Other therapies that have been reported as beneficial are parenteral gold therapy, dapsone, tetracycline, and plasmapheresis.Plasmapheresis is particularly useful in patients refractory to corticosteroids. A therapy described by Rook and colleagues involves administration of 8-methoxypsoralen followed by exposure of peripheral blood to ultraviolet radiation.
steroids must be used for long periods of time, adjuvants such as azathioprine or cyclophosphamide are added to the regimen to reduce the complications of long-term corticosteroid therapy. Prednisone is used initially to bring the disease under control, and, once this is achieved, the dose of prednisone is decreased to the lowest possible maintenance levels. Patients with only oral involvement also may need lower doses of prednisone for shorter periods of time, so the clinician should weigh the potential benefits of adding adjuvant therapy against the risks of additional complications such as blood dyscrasias, hepatitis, and an increased risk of malignancy later in life. There is no one accepted treatment for pemphigus confined to the mouth, but one 5-year follow -up study of the treatment of oral pemphigus showed no additional benefit of adding cyclophosphamide or cyclosporine to prednisone versus prednisone alone, and it showed a higher rate of complications in the group taking the immunosuppressive drug.Most studies of pemphigus of the skin show a decreased mortality rate when adjuvant therapy is given along with prednisone.One new immunosuppressive drug, mycophenolate, has been effective when managing patients resistant to other adjuvants.The need for systemic steroids may be lowered further in cases of oral pemphigus by combining topical with systemic steroid therapy, either by allowing the prednisone tablets to dissolve slowly in the mouth before swallowing or by using potent topical steroid creams. Other therapies that have been reported as beneficial are parenteral gold therapy, dapsone, tetracycline, and plasmapheresis.Plasmapheresis is particularly useful in patients refractory to corticosteroids. A therapy described by Rook and colleagues involves administration of 8-methoxypsoralen followed by exposure of peripheral blood to ultraviolet radiation.