Fibrous Inflammatory Hyperplasias and Traumatic Fibromas
FIBROMA, EPULIS FISSURATUM, AND PULP POLYP
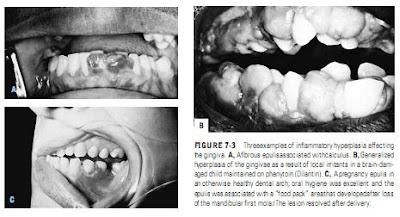
Fibrous inflammatory hyperplasias may occur as either pedunculated or sessile (broad-based) growths on any surface of the oral mucous membrane ( Figure 7-2). They are called fibromas if they are sessile, firm, and covered by thin squamous epithelium. On the gingiva, a similar lesion is often referred to as an
epulis (Figure 7-3). The majority remain small, and lesions that are > 1 cm in diameter are rare. An exception to this rule occurs with a lesion that is associated with the periphery of illfitting dentures,the so-called epulis fissuratum, in which theFIBROMA, EPULIS FISSURATUM, AND PULP POLYP
Fibrous inflammatory hyperplasias may occur as either pedunculated or sessile (broad-based) growths on any surface of the oral mucous membrane ( Figure 7-2). They are called fibromas if they are sessile, firm, and covered by thin squamous epithelium. On the gingiva, a similar lesion is often referred to as an
growth is often split by the edge of the denture, one part of the lesion lying under the denture and the other part lying between the lip or cheek and the outer denture surface. This lesion may extend the full length of one side of the denture. Many such hyperplastic growths will become less edematous and inflamed following the removal of the associated chronic irritant, but they rarely resolve entirely. In the preparation of the mouth to FIGURE 7-2 A, Pedunculated fibrous inflammatory hyperplasia of the cheek, possibly associated with dental trauma. B and C, On biopsy, a comparable soft nodular swelling of the lip proved to be a small benign growth made up of mature fat cells (lipoma). ( B and C courtesy of Gary Cohen, DMD, Philadelphia, Pa.)
receive dentures, these lesions are excised to prevent further irritation and to ensure a soft-tissue seal for the denture periphery. Pulp polyps represent an analogous condition (chronic hyperplastic pulpitis) involving the pulpal connective tissue, which proliferates through a large pulpal exposure and fills the cavity in the tooth with a mushroom-shaped polyp that is connected by a stalk to the pulp chamber. Masticatory
pressure usually leads to keratinization of the epithelial covering of these lesions. Characteristically, pulp polyps (like granulation tissue) contain few sensory nerve fibers and are remarkably insensitive. The crowns of teeth affected by pulp polyps are usually so badly destroyed by caries that endodontic treatment is not considered; however, when restorative considerations do not preclude it, root canal therapy can be satisfactorily completed on these teeth after the extirpation of the polyp and remaining pulp tissue.
The differential diagnosis of fibrous inflammatory hyperplasia should include consideration of the possibility that the lesion is a true papilloma (a cauliflower-like mass made up of multiple fingerlike projections of stratified squamous epithelium with a central core of vascular connective tissue) or a small verrucous carcinoma. Multiple oral papillomatous lesions also may be virus-induced warts (see “Benign ‘Virus-Induced’ Tumors”) or one feature of a syndrome with more serious manifestations in other organs (eg, acanthosis nigricans or ichthyosis hystrix). On the dorsal surface of the tongue, nodular lesions may represent scars, neurofibroma, and granular cell tumor as well as fibrous inflammatory hyperplasia. Both pedunculated and broad-based nodules on the pharyngeal surface of the tongue are usually lymphoid nodules or cystic dilatations of mucous gland ducts (see Figure 7-3, C). Condyloma latum, one of the characteristic oral lesions of secondary syphilis, has been reported to involve the intraoral mucosa.
Fibrous inflammatory hyperplasias have no malignant potential, and recurrences following excision are almost always a result of the failure to eliminate the particular form of chronic irritation involved. The occasional report of squamous cell carcinoma arising in an area of chronic denture irritation, however, underlines the fact that no oral growth, even those associated with an obvious chronic irritant, can be assumed to be benign until proven so by histologic study. Thus, whenever possible, all fibrous inflammatory hyperplasias of the oral cavity should be treated by local excision, with microscopic examination of the excised tissue.
PALATAL PAPILLARY HYPERPLASIA
Palatal papillary hyperplasia (denture papillomatosis) is a common lesion with a characteristic clinical appearance that develops on the hard palate in response to chronic denture irritation in approximately 3 to 4% of denture wearers.
Full dentures in which relief areas or “suction chambers” are cut in the palatal seating surface appear to be the strongest stimuli, but the lesion is also seen under partial dentures, and occasional case reports have described the lesion in patients who have never worn dentures.
The palatal lesion is usually associated with some degree of denture sore mouth (stomatitis) due to chronic candidal infection, which influences the appearance of the papillary hyperplasia. When complicated by candidal infection, the lesion may be red to scarlet, and the swollen and tightly packed projections resemble the surface of an overripe berry. Such lesions are friable, often bleed with minimal trauma, and may be covered with a thin whitish exudate. When the candidal infection is eliminated, either by removing the denture or by topical administration of an antifungal agent, the papillary lesion becomes little different in color from the rest of the palate and consists of more or less tightly packed nodular projections. If tiny, the nodular projections simply give a feltlike texture to that portion of the palate, and the lesion may even pass unnoticed unless it is stroked with an instrument or disturbed by a jet of air.
The microscopic appearance of these lesions is little different from that of “papillomas” elsewhere in the mouth although the degree of branching and polypoid proliferation that develop on the epithelial surface occluded by the denture is often quite surprising. Low-power examination of these lesions demonstrates their exophytic nature, and neither epithelial invasion of the submucosa nor resorption of the palatine bone occurs, even under large or long-standing lesions. Despite their sometimes bizarre clinical appearance, these lesions have almost no neoplastic potential, a finding that is borne out by the absence of atypia and cellular dysplasia in biopsy specimens.
If the alveolar ridges are surgically prepared for new dentures,papillary hyperplasia lesions are usually excised or removed (by electrocautery, cryosurgery, or laser surgery), and the old denture or a palatal splint is used to maintain a postoperative surgical dressing over the denuded area.
If florid papillomatosis of the palate occurs or persists in the absence of dentures, the differential diagnosis should also consider several granulomatous diseases that may manifest intraorally in this fashion (eg, infectious granulomas, Cowden disease, and verrucous carcinoma), particularly when the papillary lesions are white and extend beyond the palatal vault and onto the alveolar mucosa.