The majority of cases of lichen planus present as white lesions (discussed in detail in Chapter 5). An erosive and bullous form of this disease presents as chronic multiple oral mucosal ulcers. Erosive and bullous lesions of lichen planus occur in the severe form of the disease when extensive degeneration of the basal layer of epithelium causes a separation of the epithelium from the underlying connective tissue.In some cases, the
lesions start as vesicles or bullae—this has been classified as “bullous lichen planus”; in a majority of cases, the disease is characterized by ulcers and is called “erosive lichen planus.” Both of these disorders are variations of the same process and should be considered together. The erosive form of lichen planus has been associated with drug therapy, underlying medical disorders, and reactions to dental restorations.The drugs most commonly associated with severe lichenoid reactions include NSAIDs, hydrochlorothiazide, penicillamine, and angiotensin-converting enzyme inhibitors. The most frequently reported underlying disease associated with oral lichenoid reactions is chronic hepatitis caused by hepatitis C, particularly in Japan and the Mediterranean region.
Contact allergic reactions to flavoring agents such as cinnamon and peppermint and to dental materials such as mercury in amalgam may also result in lichenoid reactions of the oral mucosa.Lichen planus lesions suspected of being caused by contact allergy should be in direct contact with the suspected allergen. Graft-versus-host disease due to bone marrow transplantation also causes oral lichenoid lesions.
The association between erosive lichen planus and squamous cell carcinoma remains controversial. There have been many case reports of carcinoma developing in areas of lichen planus.A case by Massa and colleagues shows histologic progression from lichen planus, lichen planus with epithelial atypia, and frank squamous cell carcinoma.Reviews of large numbers of patients with lichen planus by Silverman and colleagues and Murti and associates show an association between the two diseases of between 0.4 and 1.2%.Affected patients were frequently tobacco users; this leads to speculation that lichen planus is a cofactor in malignant transformation.
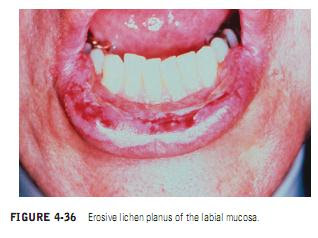
Clinical Manifestations. Erosive lichen planus is characterized by the presence of vesicles, bullae, or irregular shallow ulcers of the oral mucosa(Figures 4-36 and 4-37). The lesions are usually present for weeks to months and thus can be distinguished from those of aphthous stomatitis, which form and heal in a period of 10 days to 2 weeks. A significant number of cases of erosive lichen planus present with a picture of desquamative gingivitis(Figure 4-38). It is important to remember that desquamative gingivitis is not a disease entity but a sign of disease that can be caused by erosive lichen planus, pemphigus vulgaris, or cicatricial pemphigoid. Desquamative gingivitis caused by lichen planus may be accompanied by characteristic Wickham’s striae, simplifying the diagnosis, or they may be present without other lesions.
Diagnosis. A diagnosis of erosive lichen planus should be suspected when erosive or bullous lesions are accompanied by typical lichenoid white lesions. Biopsy is necessary for definitive diagnosis. Biopsy of the erosive lesions shows hydropic degeneration of the basal layer of epithelium. This can help to distinguish it from mucous membrane pemphigoid, which is also a subepithelial lesion but which shows an intact basal layer, or from pemphigus vulgaris, in which acantholysis is demonstrated. Direct immunofluorescence should be performed on biopsy specimens when pemphigus, pemphigoid, or discoid lupus erythematosus is included in the differential diagnosis.
Management. Patients with severe lichen planus should have drug therapy and underlying disease ruled out as possible causes. The bullous and erosive forms of lichen planus can be
distressingly painful. The treatment of choice is topical corticosteroids (Figure 4-39). Intralesional steroids can be used for indolent lesions, and, in cases of severe exacerbation, systemic steroids may be considered for short periods of time. Cyclosporine rinses may be effective for patients with severe erosions resistant to topical steroids, although the expense may be a limiting factor.Tacrolimus, another immunosuppressive drug, has recently been marketed in a topical form and has been reported useful in the management of oral erosive lichen planus. Systemic etretinate, dapsone, or photochemotherapy have also been reported to be effective in severe resistant cases.Because patients with oral lichen planus appear to be in a higher risk group for development of squamous cell carcinoma, it is prudent to periodically evaluate all patients with erosive and bullous forms of lichen planus for the presence of suspicious lesions requiring biopsy (Figure 4-40).