EM is an immune-mediated disease that may be initiated either by deposition of immune complexes in the superficial microvasculature of skin and mucosa, or cell-mediated immunity. Kazmierowski and Wuepper studied specimens of lesions less than 24 hours old from 17 patients with EM; 13 of the 17 had deposition of immunoglobulin (Ig) M and complement (C) 3 in the superficial vessels.
Other health care workers have detected elevated levels of immune complexes and decreased complement in fluid samples taken from vesicles.
Although the histopathology is not specific, two major histologic patterns have been described: an epidermal pattern characterized by lichenoid vasculitis and intraepidermal vesicles, and a dermal pattern characterized by lymphocytic vasculitis and subepidermal vesiculation.
The most common triggers for episodes of EM are herpes simplex virus and drug reactions. The drugs most frequently associated with EM reactions are oxycam nonsteroidal antiinflammatory drugs (NSAIDs); sulfonamides; anticonvulsants such as carbamazepine, phenobarbital, and phenytoin; trimethoprim-sulfonamide combinations, allopurinol, and penicillin.A majority of the severe cases of Stevens-Johnson syndrome or TEN are caused by drug reactions.
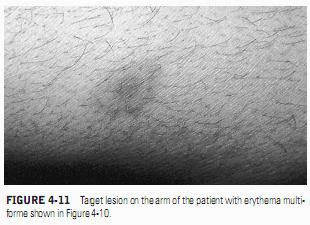
The relationship of HSV to episodes of EM has been known for over 50 years, but improved diagnostic techniques, including polymerase chain reaction (PCR) and in situ hybridization have demonstrated that herpes-associated EM is a common form of the disease, accounting for at least 20 to 40% of the cases of single episodes of EM and approximately 80% of recurrent EM(Figures 4-10 and 4-11). Herpes antigens have been demonstrated in the skin and immunocomplexes obtained from patients with EM. Many investigators now believe that the major cause of EM is a cellular immune response to HSV antigens deposited in keratinocytes of the skin and mucosa.The tendency to develop mucous membrane lesions during episodes of herpes-associated EM appears to be genetically determined and related to specific human leukocyte antigen (HLA) types.
Oral mucosal lesions were detected in 8 of 12 children with HSV-associated EM.
Other triggers for EM include progesterone, Mycoplasma benign and malignant tumors, radiotherapy, Crohn’s disease, sarcoidosis, histoplasmosis, and infectious mononucleosis.
Many cases of EM continue to have no obvious detectable cause after extensive testing for underlying systemic disease and allergy and are labeled idiopathic.