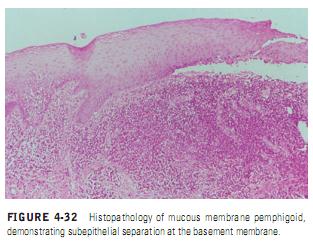
MMP is a chronic autoimmune subepithelial disease that primarily affects the mucous membranes of patients over the age of 50 years, resulting in mucosal ulceration and subsequent scarring. The primary lesion of MMP occurs when autoantibodies directed against proteins in the basement membrane zone,
acting with complement (C3) and neutrophils, cause a subepithelial split and
acting with complement (C3) and neutrophils, cause a subepithelial split and
subsequent vesicle formation (Figure 4-32). The antigens associated with MMP are most frequently present in the lamina lucida portion of the basement membrane, but recent research has demonstrated that the identical antigen is not involved in all cases, and the lamina densa may be the primary site of involvement in some cases. The circulating autoantibodies are not the same in all cases, and subsets of MMP have been identified by the technique of immunofluorescent staining of skin that has been split at the basement membrane zone with the use of sodium chloride.The majority of cases of MMP demonstrate IgG directed against antigens on the epidermal side of the salt-split skin, which have been identified as BP 180 (also called type XVII collagen); however, cases of MMP have also been identified where the antigen is present on the dermal side of the split. This latter antigen has been identified as epiligrin (laminin 5), an adhesion molecule that is a component of the anchoring filaments of the basement membrane.
Clinical Manifestations. The subepithelial lesions of MMP may involve any mucosal surface, but they most frequently involve the oral mucosa. The conjunctiva is the second most common site of involvement and can lead to scarring and adhesions developing between the bulbar and palpebral conjunctiva called symblepharon (Figure 4-33, A and B). Corneal damage is common, and progressive scarring leads to blindness in close to 15% of patients. Lesions may also affect the genital mucosa, causing pain and sexual dysfunction. Laryngeal involvement causes pain, hoarseness, and difficulty breathing, whereas esophageal involvement may cause dysphagia, which can lead to debilitation and death in severe cases. Skin lesions, usually of the head and neck region, are present in 20 to 30% of patients.
Oral Manifestations. Oral lesions occur in over 90% of patients with MMP. Desquamative gingivitis is the most common manifestation and may be the only manifestation of the disease (Figure 4-34). Since these desquamative lesions resemble the lesions of erosive lichen planus and pemphigus, all cases of desquamative gingivitis should be biopsied and studied with both routine histology and direct immunofluorescence to determine the correct diagnosis. Lesions may present as intact vesicles of the gingival or other mucosal surfaces, but more frequently they appear as nonspecific-appearing erosions (Figure 4-35). The erosions typically spread more slowly than pemphigus lesions and are more self-limiting.
Diagnosis. Patients with MMP included in the differential diagnosis must have a biopsy done for both routine and direct immunofluorescent study. Routine histopathology shows subbasilar cleavage. Using the direct immunofluorescent technique (see “Laboratory Tests” under “Pemphigus Vulgaris” for description), biopsy specimens taken from MMP patients demonstrate positive fluorescence for immunoglobulin and complement in the basement membrane zone in 50 to 80% of patients. Splitting the biopsy specimen at the basement membrane zone with 1 M NaCl prior to direct immunofluorescence increases the sensitivity of the test. The direct immunofluorescent technique is excellent for distinguishing MMP
Oral Manifestations. Oral lesions occur in over 90% of patients with MMP. Desquamative gingivitis is the most common manifestation and may be the only manifestation of the disease (Figure 4-34). Since these desquamative lesions resemble the lesions of erosive lichen planus and pemphigus, all cases of desquamative gingivitis should be biopsied and studied with both routine histology and direct immunofluorescence to determine the correct diagnosis. Lesions may present as intact vesicles of the gingival or other mucosal surfaces, but more frequently they appear as nonspecific-appearing erosions (Figure 4-35). The erosions typically spread more slowly than pemphigus lesions and are more self-limiting.
Diagnosis. Patients with MMP included in the differential diagnosis must have a biopsy done for both routine and direct immunofluorescent study. Routine histopathology shows subbasilar cleavage. Using the direct immunofluorescent technique (see “Laboratory Tests” under “Pemphigus Vulgaris” for description), biopsy specimens taken from MMP patients demonstrate positive fluorescence for immunoglobulin and complement in the basement membrane zone in 50 to 80% of patients. Splitting the biopsy specimen at the basement membrane zone with 1 M NaCl prior to direct immunofluorescence increases the sensitivity of the test. The direct immunofluorescent technique is excellent for distinguishing MMP
from pemphigus, and specimens obtained show immunoglobulin and complement deposition in the intercellular substance of the prickle cell layer of the epithelium. Only 10% of MMP patients demonstrate positive indirect immunofluorescence for circulating antibasement membrane-zone antibodies; however, use of salt-split skin as a substrate increases the sensitivity of this test.
Treatment. Management of MMP depends on the severity of symptoms. When the lesions are confined to the oral mucosa, systemic corticosteroids will suppress their formation, but the clinician must weigh the benefits against the hazards from side effects of the drug.
176
Unlike pemphigus, MMP is not a fatal disease, and long-term use of steroids for this purpose must be carefully evaluated, particularly because most cases are chronic, most patients are elderly, and treatment is required for a long period of time.
Patients with mild oral disease should be treated with topical and intralesional steroids. Desquamative gingivitis can often be managed with topical steroids in a soft dental splint that covers the gingiva, although the clinician using topical steroids over large areas of mucosa must closely monitor the patient for side effects such as candidiasis and effects of systemic absorption. When topical or intralesional therapy is not successful, dapsone therapy may be attempted. Rogers and Mehregan have developed a protocol for use of dapsone in patients with MMP.The effectiveness of this protocol for the management of MMP was recently confirmed by Ciarrocca and Greenberg.Since dapsone causes hemolysis and methemoglobinemia, glucose-6-phosphate dehydrogenase deficiency must be ruled out, and the patient’s hemoglobin must be closely monitored. Methemoglobinemia can be reduced with the use of cimetidine and vitamin E.Another rare side effect of dapsone is dapsone hypersensitivity syndrome, an idiosyncratic disorder characterized by fever, lymphadenopathy, skin eruptions, and occasional liver involvement. Patients resistant to dapsone should be treated with a combination of systemic corticosteroids and immunosuppressive drugs,particularly when there is risk of blindness from conjunctival involvement,
Treatment. Management of MMP depends on the severity of symptoms. When the lesions are confined to the oral mucosa, systemic corticosteroids will suppress their formation, but the clinician must weigh the benefits against the hazards from side effects of the drug.
176
Unlike pemphigus, MMP is not a fatal disease, and long-term use of steroids for this purpose must be carefully evaluated, particularly because most cases are chronic, most patients are elderly, and treatment is required for a long period of time.
Patients with mild oral disease should be treated with topical and intralesional steroids. Desquamative gingivitis can often be managed with topical steroids in a soft dental splint that covers the gingiva, although the clinician using topical steroids over large areas of mucosa must closely monitor the patient for side effects such as candidiasis and effects of systemic absorption. When topical or intralesional therapy is not successful, dapsone therapy may be attempted. Rogers and Mehregan have developed a protocol for use of dapsone in patients with MMP.The effectiveness of this protocol for the management of MMP was recently confirmed by Ciarrocca and Greenberg.Since dapsone causes hemolysis and methemoglobinemia, glucose-6-phosphate dehydrogenase deficiency must be ruled out, and the patient’s hemoglobin must be closely monitored. Methemoglobinemia can be reduced with the use of cimetidine and vitamin E.Another rare side effect of dapsone is dapsone hypersensitivity syndrome, an idiosyncratic disorder characterized by fever, lymphadenopathy, skin eruptions, and occasional liver involvement. Patients resistant to dapsone should be treated with a combination of systemic corticosteroids and immunosuppressive drugs,particularly when there is risk of blindness from conjunctival involvement,
or significant laryngeal or esophageal damage. Reports suggest that tetracycline and nicotinamide may also be helpful in controlling the lesions of MMP.